Bridging the Gap: Dietetic Internship Preceptors' Knowledge and Adoption of Weight-Inclusive Care
By Claire Knutson
Introduction:
Weight is not a behavior, and by treating it like one, healthcare professionals may be harming patients. Weight-centric approaches, which encourage interventions to reduce body weight and size, have long dominated healthcare professions, including dietetics, but recently evidence questions the effectiveness of intentional weight loss in improving patient health outcomes. Weight-inclusive care approaches, including Health at Every Size (HAES)TM and Intuitive Eating, have begun to shift care towards a focus on health behaviors, rather than weight. This research investigated dietetic internship preceptors’ preparedness to challenge weight-centric approaches and adopt weight-inclusive care.
Weight stigma in healthcare is well-documented and has harmful effects on individuals. From delayed diagnosis, less aggressive treatment recommendations, and increased negative assumptions, those who experience weight bias are left with poorer physical and mental health outcomes.1
Assumingthatweight loss is necessarytoimprovehealthoutcomescan perpetuateweightbiasesand stigma.Weight-inclusive care approaches focus on behaviors such as nutrition, mindful movement, sleep, and mental well-beingwhile accepting body diversity.Rather than recommending that a patient achieve a normal body weight per body mass index (BMI) measurement, weight-inclusive goals are patient-centered,behavior-focused, and do not focus on weight.
The Seven Weight Inclusive Principles:
1. Do No Harm
2. Appreciate that bodies come in a variety of shapes and sizes
3. Encourage a process-focus
4. Maintain a holistic focus
5. Evaluate weight lossresearch and applysustainable, evidence-basedpractices in care
6. Create healthful, individualized practices and environments that are sustainable
7. Support equitable care and autonomy across the weight spectrum
Breaking Down the Research:
We conducted a mixed methods survey with dietetic intern preceptors across diverse practice settings using three validated tools, the Intuitive Eating Scale (IES-3), Body Trust Scale (BTS), and Self-Compassion Scale, aiming to (1) assess preceptors’ knowledge of weight-inclusive care, (2) understand their current attitudes and use of weight-inclusive approaches, and (3) identify opportunities to support preceptors in adopting weight-inclusive care practices.
Forty-one preceptors participated in the survey, representing a 27% response rate. The results were promising, showing that 87% of dietetic intern preceptor respondents (Figure 1) felt ready to use a weight-inclusive care approach, and 86% believed that weight-inclusive approaches are important (Figure 2). We also found that intuitive eating practices and body trust were strongly correlated, as were readiness to practice weight-inclusivity and rating of its importance. Additionally, 90% emphasized sustainable, individualized health behaviors, while 98% supported body diversity and equitable care. While all seven weight-inclusive approaches were present in preceptors’ practices, 61% struggled to evaluate weight loss research critically, and 76% found it difficult to advocate for equitable healthcare access. Dietetic intern preceptors stated they believed continuing education (CPEU) training would be the most helpful way to further their knowledge of weight-inclusive care approaches.
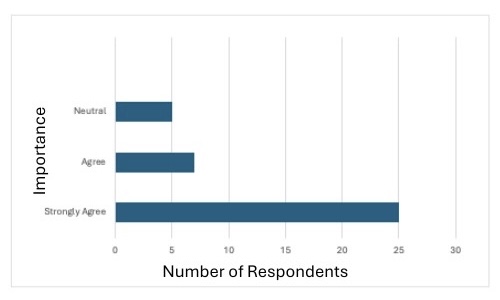 Figure 1: Preceptors' ratings of the importance of using a weight-inclusive approach.
Figure 1: Preceptors' ratings of the importance of using a weight-inclusive approach.
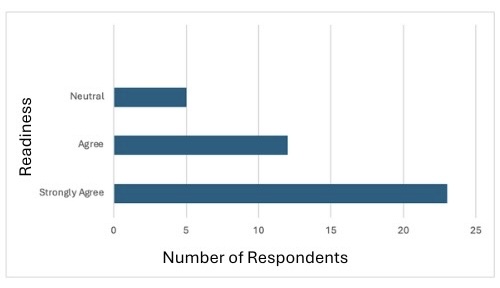 Figure 2: Preceptors' readiness to use weight-inclusive care approach.
Figure 2: Preceptors' readiness to use weight-inclusive care approach.
Implications:
Preceptors play a vital role in shaping future dietetics practice. While about one-third of preceptors were enthusiastic about weight-inclusive care, 73% did not participate in the survey. Institutions can help to reduce systemic weight bias by supporting continuing education for preceptors to introduce the concepts and advance knowledge for those who are familiar. Prioritizing weight-inclusive education during the dietetic internship may improve the quality of care, health outcomes, and accessibility of care to all.
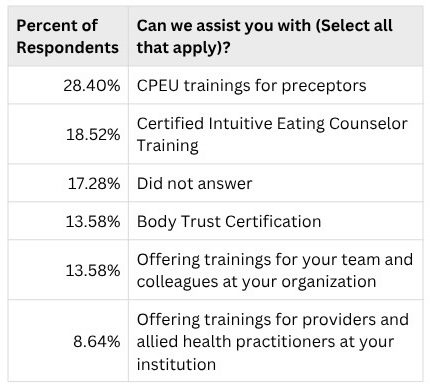 Figure 3: Needs identified by preceptors
Figure 3: Needs identified by preceptors
Conclusion:
Weight bias is a significant issue in healthcare, and addressing it requires a shift from traditional weight-centric models to a weight-inclusive care approach. Preceptors would like the dietetic internship program to provide continuing education opportunities to analyze weight-science literature and discover multi-level strategies to address weight bias in healthcare.
References:
1. Ginsburg BM, Daley SF, Sheer AJ. Overcoming Stigma and Bias in Obesity Management. Treasure Island (FL): StatPearls Publishing; 2025 Jan–. Accessed June 24, 2025. https://www.ncbi.nlm.nih.gov/books/NBK578197/
